Conditions
Hernia Repair

Mr Baskerville has run a hernia clinic at King’s College Hospital for many years, and is currently developing new techniques for improving groin hernia surgery. His hernia interests coincided with developing one of the earliest Day Surgery Centres in the United Kingdom in Kingston Surrey, after which he worked with Mr Jerry Gilmore, Hernia Expert and exponent of the surgery of Gilmore’s Groin.
What is a hernia?
A hernia (sometimes called a rupture) occurs when an organ or part of it (the lining of that organ) pokes through the sheath of muscles that surround it, usually causing a visible bump or swelling, and sometimes pain.
Groin hernias can occur in anyone at any age, but are more common in men than women. They usually occur when the muscle in the groin weakens sufficiently to allow the bowel or its lining to poke through gaps in these muscles. Occasionally a fall or a blow can tear the muscles so that the hernia develops rapidly.
The developing hernia may appear as a bulge in the groin, usually on standing or straining. In the early stages, this bulge will usually disappear when lying down.
Hernias can be painful when they first appear, but this usually settles within a few weeks. More commonly the hernia when visible is associated with a dragging, rather unpleasant sensation which is made worse when gardening, doing DIY, lifting heavy objects or straining.
Some people have these from infancy, but most will develop in adulthood, either as a result of pregnancy or as a result of general abdominal weakness.
The umbilicus starts to stick out, first of all when straining, then eventually at all times. The hernia in this case usually consists of internal fat, and repair is relatively straightforward. It is not always necessary to insert a mesh when performing the repair; other techniques may be more suitable.
Although most hernia repairs are successful, they can never make the tissues as good as new. There will always be a risk that the hernia comes back: a recurrent hernia.
The chances of recurrence increase with loss of muscle tone, increased girth or the development of a chronic cough. The risk of a groin hernia recurring is said to range from 2% to 5% over a ten year period, but may rise to 10% in some cases.
Recurrent hernias can be repaired, sometimes more than once, but the law of diminishing returns will apply. Your hernia surgeon should be able to discuss how to avoid a recurrence, and the risks of recurrences occurring.
Any operation on the abdomen requires an incision through the abdominal wall (including the muscles) in order to access the organ to be treated, such as the gall bladder, the bowel or the womb, etc. Even keyhole surgery requires these incisions, although the muscle disruption in keyhole surgery is small.
Although the abdominal structures are repaired at end of the operation, the wounds consist of scar tissue which is weaker than normal tissue. Occasionally the scar tissue breaks down and a hernia develops at the site of the incision: an incisional hernia.
These are often uncomfortable, and can vary enormously in both size and complexity. Most require repair, but some can be managed without surgery. Your hernia surgeon should be able to advise as to the best course of treatment to follow.
Given their position in the human body, it is not surprising that two of the most significant drawbacks to surgical repair of groin hernias are recurrence and the development of chronic pain at the site of the repair. Chronic pain may develop in up to 12% (1 in 8) patients following routine hernia repairs, whether performed by open surgery or using keyhole techniques. The causes of the pain are poorly understood, but much research has gone into avoiding this problem by developing new approaches to hernia repair. One of the more successful of these was the development of the pre-peritoneal repair technique of Pélissier TIPP technique) which Mr Baskerville helped develop in the U.K., and which has been associated with a significant reduction in post-operative chronic pain.
In 2011, the technique was simplified and renamed ONSTEP (Open Non SuTured Extra Peritoneal repair). Mr Baskerville and a group of hernia specialists in Europe have been developing this technique and have now treated over 1,000 patients: ONSTEP appears to combine a successful repair with little or no post-operative pain. It can be performed safely as a day case, under local anaesthesia when required. ONSTEP is also associated with a very rapid return to normal activities.
The main benefits are the relief of pain and discomfort caused by the hernia and avoidance of future obstruction (blockage) or strangulation. Strangulation occurs when part of the intestine (bowel) bulges out of the hernia defect and becomes trapped and starts getting more swollen and painful. If the hernia suddenly becomes very painful and hard, the blood supply of the contents may be in danger and will require an emergency operation to repair it.
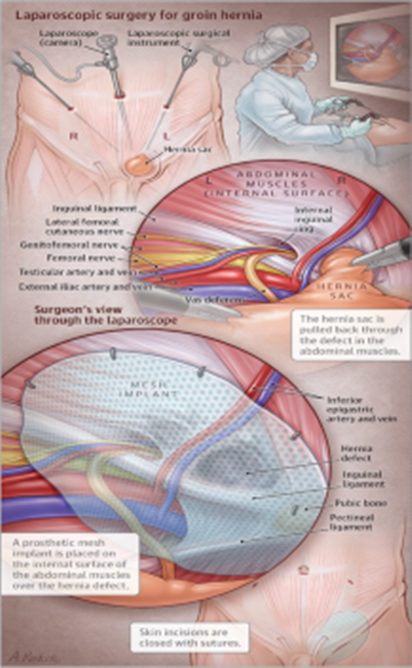 The word “Laparoscopic” means keyhole surgery and this is an operation under
general anaesthesia. Three or four small cuts (up to 1 cm wide) are made in
your tummy and thin, long instruments are passed into these incisions. One
instrument is the camera so that the surgeon can see what is happening
inside the tummy, with the added benefit of a magnified view of all the
inside parts of the tummy. The surgeon then uses thin, long delicate
instruments that fit through the 1 cm cuts, to return the protruding lump
(which forms the hernia) back into the abdominal cavity. To provide space
for the surgery to be performed, your tummy is filled with a harmless gas. A
piece of mesh (a strong, but flexible man-made material) is inserted over
the weak area in the abdominal wall to strengthen it. The mesh remains there
permanently to reinforce the weak area and is expected to get incorporated
with your own tissues. Once the operation is completed, the gas is allowed
to escape before the cuts are stitched together. Some of the gas remains and
can cause some discomfort after the operation. The faster you get up and
about and walk after the procedure the faster your recovery.
The word “Laparoscopic” means keyhole surgery and this is an operation under
general anaesthesia. Three or four small cuts (up to 1 cm wide) are made in
your tummy and thin, long instruments are passed into these incisions. One
instrument is the camera so that the surgeon can see what is happening
inside the tummy, with the added benefit of a magnified view of all the
inside parts of the tummy. The surgeon then uses thin, long delicate
instruments that fit through the 1 cm cuts, to return the protruding lump
(which forms the hernia) back into the abdominal cavity. To provide space
for the surgery to be performed, your tummy is filled with a harmless gas. A
piece of mesh (a strong, but flexible man-made material) is inserted over
the weak area in the abdominal wall to strengthen it. The mesh remains there
permanently to reinforce the weak area and is expected to get incorporated
with your own tissues. Once the operation is completed, the gas is allowed
to escape before the cuts are stitched together. Some of the gas remains and
can cause some discomfort after the operation. The faster you get up and
about and walk after the procedure the faster your recovery.
An alternative to laparoscopic hernia repair is a traditional “open” hernia repair. This involves an incision about three inches long in the lower tummy. Both types of hernia repair can be performed as day case surgery.
 Laparoscopic surgery is not suitable for everyone, particularly if you have
had previous abdominal surgery or you have other underlying medical
conditions (e.g with your lungs). The surgeon will need to assess your
suitability for general anaesthesia and your medical and surgi- cal history.
The surgeon will need to consider the nature of the hernia, whether it
affects one or both sides of the groin and whether it is your first hernia
or a re-occurrence. The National Institute for Clinical Excellence (NICE)
has reviewed this procedure and recommends that laparoscopic surgery can
be used as one of the treatment options for the repair of inguinal hernia.
You can obtain more detailed information about this procedure from their
website www.nice.org.uk. Not all surgeons undertake laparoscopic surgery and
only surgeons specially trained in these techniques will undertake
Laparoscopic Hernia Repair. Sometimes, a patient may be deemed suitable for
laparoscopy but at the operation the inside of the abdomen may look
differently than expected, in which case the operation can be completed in a
traditional open manner.
Laparoscopic surgery is not suitable for everyone, particularly if you have
had previous abdominal surgery or you have other underlying medical
conditions (e.g with your lungs). The surgeon will need to assess your
suitability for general anaesthesia and your medical and surgi- cal history.
The surgeon will need to consider the nature of the hernia, whether it
affects one or both sides of the groin and whether it is your first hernia
or a re-occurrence. The National Institute for Clinical Excellence (NICE)
has reviewed this procedure and recommends that laparoscopic surgery can
be used as one of the treatment options for the repair of inguinal hernia.
You can obtain more detailed information about this procedure from their
website www.nice.org.uk. Not all surgeons undertake laparoscopic surgery and
only surgeons specially trained in these techniques will undertake
Laparoscopic Hernia Repair. Sometimes, a patient may be deemed suitable for
laparoscopy but at the operation the inside of the abdomen may look
differently than expected, in which case the operation can be completed in a
traditional open manner.
One of the benefits of laparoscopic hernia surgery over “open” hernia surgery
is that you can usually return to work and normal activities more quickly.
There may also be a lower risk of developing persistent numbness and pain
after surgery and a smaller incidence of wound infection. (This numbness
occurs, at the wound site, after the small sensation nerves in the skin are
cut at the time of the operation). Another advantage of laparoscopic surgery
is that the surgeon can view both sides of the abdomen, so if there is a
hernia on the other side there is an opportunity to repair that at the same
time, with minimal extra time / effort invested in this.
The disadvantage of laparoscopic surgery is that there is a slightly higher
risk of injury to surrounding structures or tissues (such as the bowel,
bladder, (womb / ovaries in women) and blood vessels inside the abdomen)
than there is in traditional “open” surgery.
The surgeon will discuss all the risks and benefits of both open and
laparoscopic surgery. This will enable you to choose between the procedures
and help you to decide which is the best treatment option for you.
All surgery has some risks and complications occasionally may occur: most
complications are mild and easily resolved. Specific risks of Laparoscopic
Hernia Repair are:
• In approximately 5 in 100 cases the keyhole method does not work and
the surgeon may have to convert to a traditional “open” hernia
repair.
• There is a small risk that the instruments used in keyhole surgery
may cause damage to large blood vessels, the bladder, gynaecological
organs or the intestines. This may require further surgery to repair
the damage. This may of course delay the recovery process.
• Rarely, damage may occur to the testicular vessels, leading to
swelling, pain or shrinkage of the affected testis.
• There is a chance (up to 5 in 100) that the hernia may come back,
requiring further surgery.
• Occasionally, damage to the nerves or tissue during hernia repair
may cause long term pain or numbness. This may require further
investigation or treatment.
• There may be extensive swelling and bruising of the testicles,
scrotum and penis. Testicular pain is frequent but usually only
lasts for a short period (up to 6 weeks) after surgery.
• Occasionally, some blood or fluid can build up in the groin after
surgery (called a “seroma”) and make the area swell and feel tender.
Whilst this swelling will often settle itself with- in 3 months,
sometimes you may need another small operation to get rid of it
faster.
• Difficulty in passing urine shortly after surgery may occur,
especially in men who normally wake up at night to pass urine (or
know that they have a large prostate) requiring the temporary
insertion of a catheter to empty the bladder.
• A hernia may develop around one of the wound sites. This may require
corrective surgery.
The risks of your surgery will be unique to you, depending on your previous
history of surgery and health reserves, so do not hesitate to discuss your
particular situation with your Consultant.
There is no acceptable medical treatment for a hernia, apart from surgery. A hernia does not get better over time, nor will it go away by itself. It may stay the same or most likely will grow with time. If it upsets your quality of life or you are worried about it, these are issues that would influence the decision towards repair.
As this is a day case procedure you will be expected to go home on the day of your surgery, depending on the time of the operation. For example, if your operation starts in late after- noon you will go home the next day. If you do not have nausea, can manage to walk unaided, tolerate food and drink and manage to empty your bladder then these are good indications that you can go home! Your pain will most certainly be controlled with simple painkillers, such as paracetamol or ibuprofen.
It is normal to experience some pain and soreness around the incision sites, particularly over the first few days. Your ribs will feel a bit strained (due to the mechanical ventilation dur- ing surgery) and your shoulder / neck region may also ache (irritation due to the gas in the abdomen). It is, therefore, important for you to take painkillers regularly over the first two to four days (but remember you should not exceed the stated maximum daily dose). After your discharge if the level of pain is not controlled you should consult your surgeon. You may notice some discomfort for several weeks after the operation. On rare occasions, a more chronic discomfort may persist. Whilst the full reasons for this are not known, it may, among other things, be a result of nerve damage. This may require further investigation or treatment.
You can remove any dressings five days after your surgery. You may then shower (NOT bathe) as required. If you notice that the wounds become increasingly swollen, red, painful, or if a discharge develops, arrange to see your Practice nurse or GP. It is quite common after hernia repair for men to notice marked swelling and bruising of the scrotum and penis. This will subside over a couple of weeks. If this occurs, it is advisable to wear supportive tight underwear. As the wounds heal, you may notice a numb area below the wounds. This may be due to disturbance to the nerves during surgery. Whilst in most cases sensation will gradually return, the numbness may be permanent.
Yes, you can return to your normal diet as soon as you are ready. You may feel bloated or constipated for a few days. You may experience occasional feelings of nausea (sickness) and loss of appetite over the first week or so. Eating a high fibre diet and increasing your fluid intake will help to maintain a regular bowel movement. You should normally open your bowels within 2-3 days of your operation although this may be uncomfortable at first. If you do feel you are becoming constipated mild laxatives should help. As previously mentioned, you can take measures in the week leading to your surgery to minimise these issues.
You can return to normal physical and sexual activities when you feel comfortable (variable 2-6 weeks). You can undertake gentle activities immediately after the operation if it feels comfortable to do so. You should gradually increase your level of activity, back to normal for you, over the next few weeks. If you experience an increase in pain it may be because you have done too much.
You should avoid driving for at least seven to ten days. Before driving you should ensure that you are able to perform an emergency stop, have the strength and capability to control the car, and be able to respond quickly to any situation that may occur. Please be aware that driving whilst unfit may invalidate your insurance.
You can return to work as soon as you feel well enough. Depending on how you are feeling and the type of job that you do, you will generally need about 7-14 days off work. If you have a job that involves heavy lifting or strenuous activity you may need at least 4-6 weeks off work.
• If you develop a fever above 38.0° C) or chills.
• Persistent vomiting or nausea (feeling sick).
• Increasing tummy pain or progressively worsening tummy distension.
• Increasing pain, redness, swelling or discharge from any of the wound sites.
• Significant bleeding from the wounds or difficulties in passing urine.